
Fecal Incontinence and Constipation After Stroke
Constipation and fecal incontinence affect patients at all ages and stages of life, but for those who have suffered a stroke, these conditions can have an ongoing impact on comfort, autonomy, and risk of more serious health complications.
Stroke is the third most common cause of death in the United States, after heart disease and cancer. There are approximately 795,000 new stroke cases in the US each year, leading to roughly 140,000 annual fatalities. It is also the most common cause of severe physical disability.
While aging increases stroke risk, nearly 25% of strokes occur before age 65. The risk of having a stroke more than doubles each decade after age 55.
Stroke Symptoms
There are two main types of strokes:
- Ischemic stroke occurs when a blood clot blocks the blood flow in an artery within the brain.
- Hemorrhagic stroke occurs when a blood vessel bursts within the brain.
The most common symptoms of a stroke include quick onset of:
- numbness or weakness in the face, arm, or leg, especially on one side of the body.
- vision trouble in one or both eyes.
- dizziness, difficulty walking, poor coordination and/or loss of balance.
- slurred speech, difficulty speaking, or trouble understanding speech. confusion, trouble speaking, or difficulty understanding speech.
- severe headache without any obvious cause.
The Brain-Gut Axis
After a stroke, up to 50% of patients experience GI complications, including constipation and fecal incontinence, due to the disruption of the brain-gut axis that occurs with cerebral injury.
There is a growing link between the gut and cardiovascular disease. Brain injuries, particularly stroke, have been well established as a cause of GI disorders and recently vice versa. Stroke patients associated with GI complications often have poor outcomes, with increased mortality rates and deteriorating neurologic function.
In 2010, a neuroscientist in North Carolina discovered the Enteric Nervous System, a network of neurons that is practically a brain unto itself. The brain–gut axis or gut–brain axis is often referring to the bidirectional communications between the central nervous system (CNS) and the gastrointestinal (GI) tract (microbiota and immune system).
Thus, constipation can be affected by lesions of the central and peripheral nervous systems. After a stroke, lesions in the cerebral cortex, basal ganglia, brain stem, cerebellum, and lower cranial nerves may result in constipation.4
Bowel Problems After Stroke
A considerable proportion of stroke patients suffer from gastrointestinal complications, including dysphagia, gastrointestinal hemorrhage, and constipation.
Depending on the changes in the central and peripheral nervous systems, and enteric nervous system, the transit time through the small and large intestines can be delayed, and result in incomplete bowel movements.
An effective bowel program for stroke patients is an essential component of a person’s quality of life and freedom.
Types of Bowel Incontinence
Fecal incontinence is the inability to control bowel movements, causing stool to leak unexpectedly from the rectum.
Types of fecal incontinence include:
- Anal Incontinence – involuntary loss of feces, flatus, and/or mucus.
- Flatus bowel incontinence – the sensation of a full rectum. The inability to decipher between stool and flatus leads to unexpected accidents.
- Mucus incontinence – mucus leaks due to the bowel being too full. This can be caused due to loss of feeling in the lower abdomen/perineal area, or difficulty in emptying the bowels effectively.
- Fecal incontinence – involuntary loss of feces.
Stroke-Related Fecal Incontinence
Fecal incontinence (FI) is common after a stroke. Approximately 40% of patients experience FI immediately and 10-19% of patients six months after a stroke. A stroke can cause a decrease in sensation and coordination of the rectum’s autonomic reflex system, causing the inability to control bowel movements.
Fecal incontinence among elderly people living at home was more frequent in those with a stroke. Many more incontinent stroke patients receive permanent nursing home placements than continents.
Risk factors for fecal incontinence in stroke include:
- The need for help using the toilet
- Intake of anticholinergic drugs
- Constipation and consequently constipation with overflow
Fecal Incontinence is strongly linked to:
- Older Age
- Larger Stroke
- Greater Comorbidity
- Poorer Function in Daily Activities
While FI can be treated through a variety of methods, including medications, surgery, and use of a catheter, a bowel training program is essential for the long-term health and wellness of a patient.
Constipation After a Stroke
Constipation is also a common ambulatory digestive disease diagnosis, characterized by reduced stool frequency, difficulty passing stool, or both. The main criterion for diagnosed constipation is that the symptoms have persisted for more than three months.
These symptoms include:
- Fewer than 3 spontaneous bowel movements per week
- Straining during of at least 25 percent of the bowel movements
- Lumpy or hard stools at least 25 percent of the time
- A sensation of incomplete evacuation at least 25 percent of the bowel movements
- A sensation of obstruction or blockage for at least 25 percent of bowel movements
- Manual maneuvers to help at least 25 percent of bowel movements
Causes of post-stroke constipation include:
- Inactivity
- Lethargy
- Insufficient water or nutrition intake
- Depression
- Lack of exercise capabilities
- Cognitive impairment
- Reduced consciousness and drug intake.
- Bowel microbiota disruption
Treating Post-Stroke Constipation and Incontinence
It is important to put your stroke patients who are having bowel issues on a bowel care program. ENEMEZ® can help.
Oral laxatives do not remove the contents of the sigmoid colon and rectum at a scheduled time, ENEMEEZ® does. ENEMEEZ® provides a reliable, safe, and predictive bowel movement within 2-15 minutes by providing a complete emptying of the sigmoid colon down to the rectum.
The very same product which relieves constipation, may help with fecal incontinence using a bowel program/training establishing a goal of consistent and acceptable continence.
ENEMEEZ® and Post-Stroke Constipation and Incontinence
The ENEMEEZ® formulation acts as a hyperosmotic, stool-softening laxative that works by drawing water into the bowel from surrounding body tissues used to treat general constipation and incontinence. The docusate sodium in this mini enema product prepares the stool to readily mix with watery fluids. It softens and loosens stool and initiates a normal, replicated bowel movement in a timely manner.
ENEMEEZ® Plus is the same formulation as ENEMEEZ®, with the addition of 20mg of benzocaine, assisting in the anesthetization of the rectum and lower bowel. This formulation was developed for patients who experience autonomic dysreflexia, hemorrhoids, anal fissures, or painful bowel movements.
ENEMEEZ® Versus Competing Products
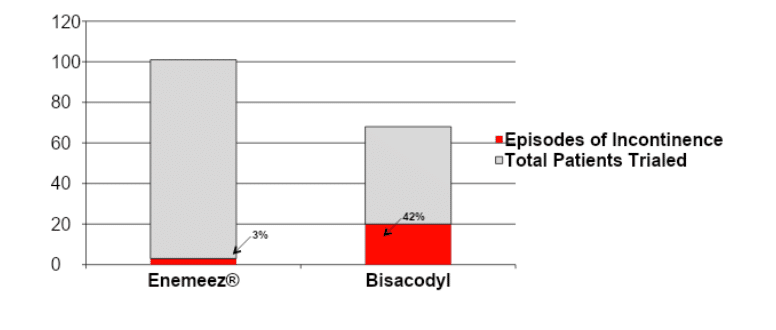
In a case study6 ENEMEEZ® mini-enema users had less than half of the incontinence episodes as compared to the competitor using Bisacodyl suppositories, and provided an evacuation in 35 minutes compared to 75 minutes with the competing product.
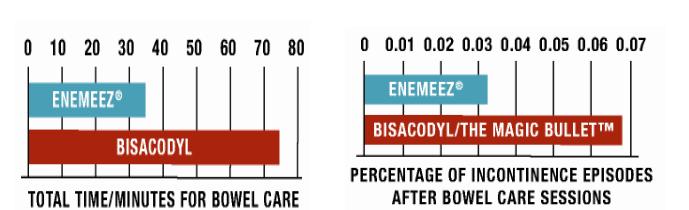
42% of Bisacodyl users experienced at least one episode of incontinence when using a suppository, whereas that number drops significantly, to only 3%, when using ENEMEEZ® mini-enemas.
Advantages of Using ENEMEEZ® in your Facility
The advantages of using ENEMEEZ® mini-enemas as bowel care for post-stroke constipation and incontinence are as follows:
- May reduce nursing intervention required for in-patient bowel care, and can result in labor cost savings to the facility.1
- May assist in the improvement of patient care and FIM scores associated with bowel care.1
- May assist with facility savings on pads, laundry, gowns, sheets, etc. due to incontinence or fecal discharge.1
- No side effects that interfere with narcotic or chemotherapy medications. Easy rectal usage for patients with pharyngeal reflex, nasogastric tube or nausea.1
- May assist in reducing time missed in therapy/rehabilitation due to episodes of incontinence, prolonged bowel care, or fatigue.1
- May reduce time spent with patients for dressing/redressing due to episodes of incontinence or fecal discharge.1
- Fast, predictable results typically in 2-15 minutes, non-irritating formula. No afterburn.1
Request ENEMEEZ® mini enema samples or an educational In-Service for your facility today.
Disclaimer: The material contained is for reference purposes only. Quest Healthcare, A Division of Quest Products, LLC, does not assume responsibility for patient care. Consult a physician prior to use. Copyright 2023 Quest Healthcare, A Division of Quest Products, LLC.
Sources:
- Bliss DZ, Johnson S, Savik K, Clabots CR, Gerding DN. Fecal incontinence in hospitalized patients who are acutely ill. Nurs Res. 2000;49(2):101–8
- Dennison C, Prasad M, Lloyd A, Bhattacharyya SK, Dhawan R, et al. (2005) The health-related quality of life and economic burden of constipation. Pharmacoeconomics 23 5: 461–76.
- National Center for Chronic Disease Prevention and Health Promotion , Division for Heart Disease and Stroke Prevention
- Krogh K, Christensen P, Laurberg S. Colorectal symptoms in patients with neurological diseases. Acta Neurol Scand 2001;103:335–43.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5484225/pdf/medi-96-e7225.pdf
- Case Study: Glen House, J, & Stiens, S. Pharmacologically initiated defecation for persons with spinal cord injury: effectiveness of three agents. Arch Phys Med Rehabil, 78, 1062-106
- Stroke Awareness Foundation
- New-Onset Fecal Incontinence After Stroke | Stroke (ahajournals.org)




![[Live Webinar] Neurogenic Bowel Dysfunction in Multiple Sclerosis](https://www.questhealthcare.net/wp-content/uploads/2025/02/325-Quest-Healthcare-Speaker-Session-1-500x383.png)


